Maternal Mortality in India: Trends, Causes, and Government Initiatives
Maternal Mortality in India: Trends, Causes, and Government Initiatives
Introduction
Maternal health is a critical indicator of a country’s overall healthcare system and societal well-being. The maternal mortality rate (MMR) measures the number of maternal deaths per 100,000 live births caused by complications during pregnancy and childbirth. Globally, maternal mortality remains a pressing public health issue, with over 700 women dying daily from preventable pregnancy-related causes, according to the World Health Organization (WHO, 2023). India has made significant strides in reducing maternal deaths over the past decades, yet disparities persist across regions and socio-economic groups. While states like Kerala historically reported very low MMR, recent data indicate a concerning rise. Understanding the trends, causes, and government initiatives is vital for devising effective strategies to ensure safe motherhood.
Understanding Maternal Mortality Rate
The Maternal Mortality Rate is a standard health indicator used to assess the safety of pregnancy and childbirth. It calculates the number of women who die due to pregnancy-related complications per 100,000 live births within a given period. MMR is influenced by a range of factors including access to skilled healthcare, nutrition, sanitation, and timely medical intervention. Unlike general mortality indicators, MMR specifically reflects the health system’s capacity to provide maternal care. Monitoring MMR over time helps policymakers identify vulnerable populations, regional disparities, and the effectiveness of health programs aimed at reducing maternal deaths.
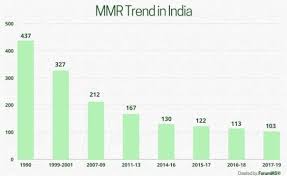
Recent Trends in India
India has witnessed a steady decline in MMR over recent years, reflecting improvements in healthcare infrastructure, institutional deliveries, and maternal care services. According to the Office of the Registrar General and Census Commissioner of India, the national MMR decreased from 103 per 100,000 live births during 2017-2019 to 93 in 2019-21. Despite this progress, certain states continue to face alarmingly high maternal death rates. For instance, Madhya Pradesh reports an MMR of 175, Assam 167, and Uttar Pradesh 151 per 100,000 live births. Odisha, Chhattisgarh, West Bengal, and Haryana also exhibit figures above the national average, indicating persistent regional disparities. Interestingly, Kerala—a state traditionally known for low maternal mortality—saw an increase from 18 to 30 per 100,000 live births between 2021 and 2023, signaling the need for renewed focus even in relatively advanced regions.
Regional Disparities and Contributing Factors
The stark variation in MMR across Indian states can be attributed to multiple factors. High maternal mortality is often concentrated in low- and lower-middle-income regions, where access to healthcare is limited. In states like Madhya Pradesh and Assam, rural populations face significant barriers including poor transportation, lack of skilled health personnel, and inadequate medical facilities. Socio-economic challenges, such as poverty, low literacy rates, and gender-based disparities, further exacerbate risks. Cultural practices, early marriage, and preference for home deliveries without skilled attendance also contribute to maternal deaths. Conversely, states with better healthcare infrastructure, higher literacy, and widespread institutional deliveries tend to report lower MMR, demonstrating the direct correlation between maternal care accessibility and survival outcomes.
Major Causes of Maternal Death
Maternal deaths are largely preventable when timely and appropriate medical care is provided. Globally, over 700 women die every day from pregnancy and childbirth-related complications, with nearly one death occurring every two minutes. In India, the key causes include severe bleeding during and after childbirth, infections, complications from unsafe abortions, and hypertensive disorders. Delays in receiving medical care—due to distance, transportation, or lack of awareness—significantly increase mortality risk. Additionally, a shortage of skilled healthcare professionals and under-resourced health facilities in rural areas contributes to preventable deaths. High-risk pregnancies, including those among adolescent mothers or women with pre-existing medical conditions, further increase vulnerability. These factors highlight the need for both systemic healthcare improvements and community-level awareness initiatives.
Government Initiatives to Reduce Maternal Mortality
India has launched multiple flagship programs to reduce maternal mortality and improve maternal health outcomes. One such initiative is the Pradhan Mantri Surakshit Matritva Abhiyan (PMSMA), which ensures quality antenatal care on a fixed day each month for all pregnant women, focusing particularly on high-risk pregnancies. The Janani Suraksha Yojana (JSY) promotes institutional deliveries by providing financial incentives to women giving birth in government facilities, aiming to reduce home births and improve maternal survival. Ayushman Bharat – Health and Wellness Centres offer comprehensive primary healthcare services, including maternal and child health, nutritional counseling, and immunization. POSHAN Abhiyaan addresses maternal malnutrition by targeting both pregnant women and children, ensuring adequate nutrition to prevent pregnancy complications. Together, these initiatives have contributed to a downward trend in MMR and enhanced maternal care coverage, though challenges in implementation remain in some regions.
Emerging Challenges and Areas for Improvement
Despite the significant progress, several challenges persist in achieving optimal maternal health outcomes. First, infrastructural gaps in rural and remote areas continue to hinder access to timely medical care. Second, the quality of maternal health services can vary widely, even within states reporting lower MMR. Third, socio-cultural barriers, including gender inequality, early marriage, and lack of awareness regarding maternal health, remain pervasive. Additionally, regional disparities in health workforce distribution, emergency transport, and availability of essential medicines exacerbate maternal risk factors. Addressing these issues requires a multi-pronged approach combining healthcare system strengthening, community engagement, and effective monitoring of maternal health programs.
The Way Forward
Ensuring safe motherhood in India demands sustained and coordinated efforts across government, civil society, and local communities. Expanding access to skilled birth attendants, emergency obstetric care, and high-quality healthcare facilities in underserved regions is critical. Strengthening community-based health awareness programs can educate women and families about the importance of institutional deliveries, antenatal care, and nutrition. Technology-driven solutions, including telemedicine and mobile health applications, can enhance maternal care in remote areas. Additionally, monitoring and evaluation mechanisms must be strengthened to identify gaps in service delivery and track progress toward reducing maternal mortality. Integrating maternal health initiatives with broader socio-economic development, such as education and women’s empowerment, will create long-term impact and reduce health inequities.
Conclusion
Maternal mortality remains a key challenge for public health in India, reflecting both the strengths and weaknesses of the healthcare system. While India has made remarkable progress in reducing MMR over the years, disparities across states, socio-economic groups, and regions persist. Understanding the causes of maternal deaths, from medical complications to socio-cultural and infrastructural barriers, is essential for designing effective interventions. Government programs such as PMSMA, JSY, Ayushman Bharat, and POSHAN Abhiyaan have demonstrated positive results, but continued efforts are needed to ensure equitable access to quality care. Addressing maternal mortality is not only a health imperative but also a vital step toward sustainable development, gender equality, and the well-being of future generations. By investing in maternal health, India can ensure safer pregnancies, reduce preventable deaths, and move closer to achieving universal health coverage and social justice.